Pain And Childbirth: Pain Relief Measures

During pregnancy, many fears and concerns arise that change over the course of the months. Towards the end of the pregnancy, pain and childbirth begin to go hand in hand. The fear of pain or complications in childbirth tends to become the protagonist.Our ancestors have given birth and, therefore, we are here, but now pain and childbirth seem to always go together.
This does not mean that we should not benefit from advances in medicine that have led to a change in the way of giving birth, but always without forgetting that all women are prepared and trained to give birth, and that pain relief techniques should be used to This is to alleviate pain, and not to medicalize childbirth and take away from women the innate power to give birth that they possess, here and now, or in the middle of the jungle and a million years ago.
Perhaps the best known, most widely used technique and the one that produced the greatest change in deliveries is epidural analgesia. It is true that it alleviates pain in labor, during labor and delivery, but we must remember and be aware that this relieves, not nullifies.
The woman must be able to feel the contractions, so that they are tolerable, but it is important that a total blockage does not occur, since this is related to higher rates of instrumented deliveries (forceps, suction cups…).
It is important to erase the idea that giving birth is not going to hurt me because I will get an epidural, and the opposite idea that giving birth will be the worst pain in the world. Each body is different, even each birth in the same woman is different, and that is what we must always remember: our birth is only ours.
During dilation and delivery, we have many options. These options can be divided into non-pharmacological and pharmacological techniques.
Pain and childbirth: non-pharmacological measures
- Relaxation and breathing techniques. The environment must be calm. Ideally, you should always be accompanied by the same midwife, so that there is a relationship of trust, that you have intimacy and a comfortable and pleasant environment. The old infrastructures of some hospitals in which more people can pass through the delivery room than in Gran Vía, the shift changes or the trainees who will witness your delivery do not help this. Remember that they should always ask your permission and introduce themselves.
- Immersion in water. Some hospitals have a birthing tub. Several studies show that immersion in water during dilation reduces the pain of contractions, benefits dilation and the tears that occur in the delivery are minimal. The problem here is that not all hospitals have a bathtub and, although some do, their staff is not trained, so they will not attend deliveries in water.
- Mobility and freedom. It is important that you can move, that you adopt the posture that is most comfortable for you, that you use the Pilates ball or Swiss ball, which allows you to perform larger movements with the pelvis that, in addition, will help the baby, lianas or any instrument that helps you . Many times, the need to maintain continuous fetal monitoring or medication pumps interferes with this freedom of movement.
- Massages, aromatherapy, hypnosis, music therapy, TENS (Transcutaneous Electrical Nervous Stimulation), application of heat and cold … Anything that helps you is useful.
Pharmacological measures
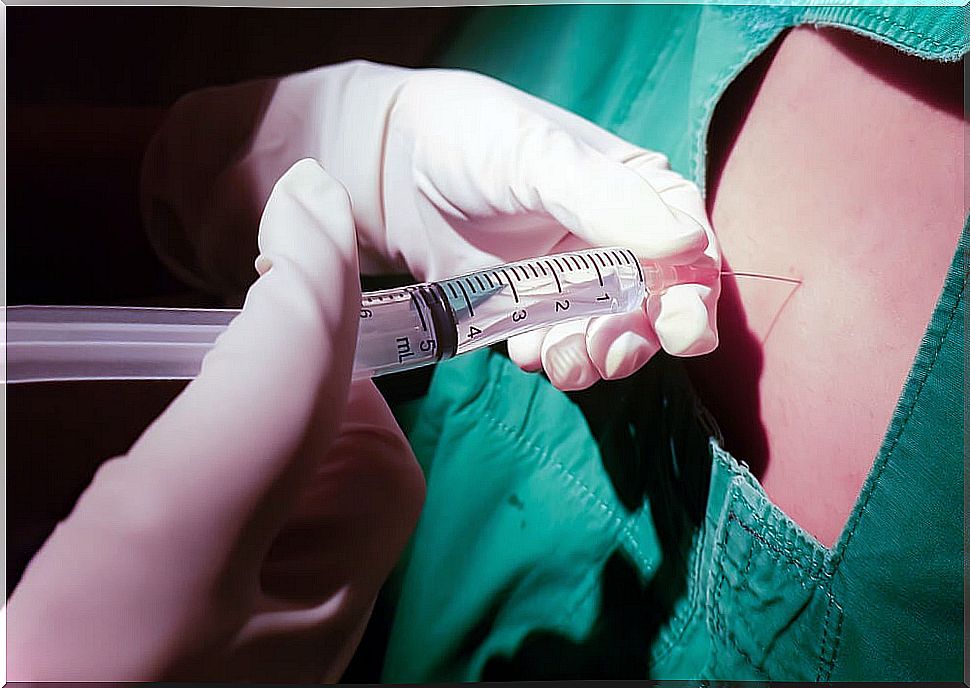
- Neuraxial block. Epidural and spinal (also combined). Epidural analgesia was discovered in 1921. It consists of introducing local anesthetics into the epidural space, which blocks the nerve endings that leave the spinal cord. They will perform a puncture in the lumbar vertebrae, where they will insert a catheter that will allow this perfusion to be maintained until the end of labor. Therefore, it is important to remember that the epidural does not wear out. It will take about 20 minutes to do a full effect. A good option is the walking epidural, which relieves pain but does not block, so you can walk and move freely. Epidural analgesia is not without risks. Before administering it, the staff in charge will inform you of this and you must sign a consent. The main risks are hypotension, back pain, itching, post-puncture headache and, in rare cases, permanent nerve damage, respiratory compromise and death.
- Peripheral blockages. Paracervical and pudendal. Paracervical block is used only in the initial phases of dilation. It has a rapid onset but more risk of side effects. The pudendal block is used in instrumented delivery, delivery, episiotomy, and sometimes as an adjunct to epidurals.
- Nitrous oxide. It is an inhaled gas. It has a rapid onset of action (about 50 seconds). It can be used in any phase of labor. It is eliminated quickly and does not affect the baby. Its effectiveness is highly variable from one person to another. It can cause nausea and dizziness that are quickly reversible when you stop using it.
In conclusion, the most important thing is that you know all the options offered by the place where you are going to give birth before delivery, as well as that you do not have a closed plan about what you want, since during the process events may arise that make you modify your plan, and this can be frustrating. It is best to know all the options and decide as the delivery progresses.